Comitiva de Promoción del Sector Salud en Las Vegas, NV USA
El Baja Health Cluster formo parte de la Comitiva de Promoción del Sector Salud que visito Las Vegas, acompañando al...

The 2019-2020 flu season officially started on October 1. Although it is early, we can get some hints of what’s to come by looking at Australia whose winter just ended. The flu season started earlier than usual there and was severe. The vast majority of the cases reported were from Influenza A. The predominant strain was H3 N2 (more on that later).
The Center for Disease Control’s FluView Activity Update tracks flu prevalence data. Currently, they report that the level of flu activity across the U.S. is low. However, deaths have already been reported including a child in California.
It is important to point out that NOW is the time to get your annual flu shot. In fact, the CDC recommends that everyone 6 months and older get a flu shot by the end of October.
To help you get through this year’s flu season, we’ve pulled together the answers to the most commonly asked questions about influenza, its prevention, and its treatment.
Flu is a self-limited acute respiratory illness that is caused by the A or B viruses of the influenza family. It occurs mainly during the cold months of the year.
Symptoms of the flu characteristically come on suddenly and typically include:
Symptoms can vary, however, ranging from being more like a cold to mainly being systemic (fever, malaise). Older individuals, in particular, may only have subtle indicators of the infection, such as weakness, loss of appetite or dizziness.
People often confuse the flu with other viral diseases like colds and viral gastroenteritis (also called ‘stomach flu’). A cold is an upper respiratory viral illness characterized by a runny nose, congestion, sneezing, sore throat, mild body aches, and sometimes mild headaches and a low-grade fever.
Colds don’t usually cause high fever or significant headaches. The flu hardly ever causes gastrointestinal symptoms in adults. They can occur, however, in about 10-20% of children. The so-called stomach flu is not flu at all, rather it is a viral gastroenteritis unrelated to infection with an influenza virus
A large retrospective study showed that when influenza was known to be going around in a community, the presence of both a cough and fever within 48 hours of developing symptoms was a strong indicator of flu (positive predictive value – 79%). The presence of sneezing makes the diagnosis of flu less likely.
In the midst of a documented flu outbreak, flu may be diagnosed based on the presence of characteristic symptoms without obtaining a lab test.
If there is a clinical need to make a definitive diagnosis, there are laboratory tests that can detect the presence of the virus in a nasal or throat swab sample. Some of these tests can be performed in the doctor’s office with results usually available within an hour. These tests may not be sensitive enough to detect all cases of flu, however. When that happens, you could still have the infection even though the rapid flu test is negative. This is called a false negative.
Other tests require the sample to be sent to a specialized lab. They take longer to get the results (hours to days) but these tests are more sensitive. Further, they may be able to determine the specific strain of the virus you are infected with.
The symptoms of the flu usually last about 3-7 days although residual malaise that interferes with the ability to exercise or do heavy work can last up to a week or more. When moderate to severe symptoms persist longer than these timeframes, it may suggest a complication such as pneumonia.
Transmission of the virus is via droplets that are spread via sneezing and coughing.
People usually become contagious about a day before symptoms start and last until about 5-7 days after you start feeling sick. There is considerable variability, however.
Children shed virus longer than adults. Further, older people, immunocompromised people, and those with chronic diseases, like chronic lung disease or diabetes, may shed for a longer period of time.
Contact with surfaces contaminated with respiratory droplets may also be a source of spread for about 24 hours.
One thing you should do if you get the flu is to stay at home when you are sick so that you don’t spread it to others. To avoid spreading the flu to family members or others if you have to go out, use a face mask and wash your hands frequently, particularly if you rub your nose, sneeze, or cough.
Be sure to keep doorknobs and counters clean as the flu virus can persist on hard surfaces for up to 24 hours. They only survive about 15 minutes on tissues.
The primary treatment of the flu is aimed at reducing symptoms. This includes the following:
A variety of antiviral drugs are available for treatment and prevention of influenza:
Although the CDC reports that the majority of viruses tested for resistance to the neuraminidase type of antiviral medications, do indeed show sensitivity – at least as of last season. It is important to note that the impact of these drugs, however, is relatively modest.
If they are started within the first 24-48 hours of the onset of symptoms, they may reduce the duration of the flu by a half-day to three days. Studies suggest that antiviral therapy also reduces the incidence and severity of complications and length of stay of people, such as older adults, who require hospitalization. Some question if there is any benefit of these drugs for healthy, immunocompetent individuals. The CDC states that “most people who are otherwise healthy and get the flu do not need to be treated with antiviral drugs.”
The Infectious Disease Society of America (IDSA) and the CDC recommend that individuals with evidence of pneumonia or severe disease that requires hospitalization be treated with an antiviral as promptly as possible. In addition, people with high-risk conditions (see below) should also be treated.
The best way to avoid getting the flu is to get an annual flu shot. The Centers for Disease Control and Prevention (CDC) recommends that everyone 6 months and older, including pregnant women, should receive the flu shot every year – preferably early in the season – unless they have a specific contraindication to any component of the influenza vaccine.
Allergy to eggs is no longer considered a contraindication. A quadrivalent vaccine, Flucelvax Quadrivalent, is grown in mammalian cells instead of egg is available in the 2019-2020 year and can be used to vaccinate individuals 4 years and older with egg allergy.
The effectiveness of the vaccine depends on how well the vaccine matches the strains of influenza circulating in that year. When there is a good match, vaccine effectiveness ranges between 40-60%. It is important to understand that even when the match is poor, the vaccine has been shown to reduce the risk of hospitalization and death from influenza.
Depending on the year, there are a variety of vaccines available including inactivated influenza virus vaccines that contain either three (Trivalent Vaccine) or four (Quadrivalent Vaccine) different flu antigens (a mix of type A and B strains). Recombinant vaccines are manufactured using recombinant DNA technology that does not require the use of the influenza virus or chicken eggs.
All of the vaccines being used in the U.S. in the 2019-2020 season, including recombinant and cell-based vaccines are quadrivalent.
The live attenuated nasal spray vaccine (FluMist) is on the recommended list this year. Here’s a link to more detailed information about that vaccine.
Although you can be vaccinated at any time during the flu season or while the flu virus is circulating in your community, you should try to get vaccinated early because it takes about 2 weeks for vaccine-induced antibodies to reach their maximum level.
The CDC recommends that everyone 6 months and older get a flu shot by the end of October.
Although antibody levels fall in the months after vaccination, revaccination during a single flu season is not recommended. It is also not harmful.
Although sporadic cases of flu are reported year-round, in North America, the season is usually considered to start in October and run through March, with the peaks in December and February. Some cases can occur as late as May.
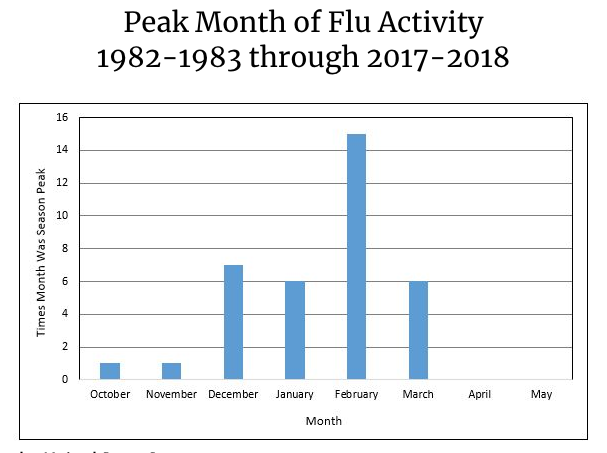
The exact timing is different depending on where in the country you live.
There are online flu trackers that you can check to see if the flu is present in your part of the country or the world. The CDC’s Weekly Influenza Map tracks the flu by state and territory and is updated weekly based on reports from epidemiologists. The World Health Organization’s (WHO) FluNet tracks circulating flu and reports the results by country.
Flu Near You publishes a map based on reports of flu-like symptoms from people all over the country. It provides a helpful overview even though the flu cases have not been verified via laboratory tests. Anyone can sign up to be a flu symptom reporter. It only takes a few minutes every week.
It is easiest to understand why annual flu shots are needed if we understand that a notable characteristic of flu viruses, particularly type A, is the changeable nature of glycoproteins that reside on the surface of the virus.
The two most important glycoproteins are hemagglutinin (H) and neuraminidase (N). There is a reason why you should know about them. The H and N glycoproteins serve as antigens to which the body forms antibodies to help fight off the infection.
We need to get vaccinated every year because these antigens change frequently. A number of different viral strains circulate each flu season. The names of the A viruses identify the variants of their glycoproteins (for example, A/H1N1 or A/H3N2).
Public health organizations, like the Center for Disease Control (CDC) and the World Health Organization (WHO) do surveillance to determine which viruses are likely to be in circulation each flu season. Every year, vaccine manufacturers use this information to create vaccines that target those variants.
But as noted above, this is not an exact science. Mismatches can occur leaving vaccinated individuals with somewhat less protection compared to years when there is a good match.
There is now a concerted effort to develop a universal vaccine. To do this scientists target antigens on the part of the virus called the stem. This is the part of the virus that doesn’t change very much. A variety of approaches are being used and some of them are now in clinical trials to determine their effectiveness. Hopefully, within the next few years, there will be a flu vaccine that can last for years similar to many of the other vaccinations that we get as children
As mentioned, the World Health Organization convenes a flu strain selection committee twice a year. The committee reviews surveillance data to determine which strains most likely to circulate during the upcoming flu season.
There is a meeting in February to determine the strains for the Northern Hemisphere and another in late September to determine strains for the Southern Hemisphere. These decisions are used to decide which strains should be included in the vaccines for that flu season.
Based on the Committee’s determination, the strains that were expected to circulate in the U.S. and which are targeted by the 2019-2020 vaccines include the following:
A/Brisbane/02/2018 (H1N1)pdm09-like virus.
A/Kansas/14/2017 (H3N2)-like virus.
Both B/Victoria and B/Yamagata virus components from the 2018-2019 flu vaccine remain the same for the 2019-2020 flu vaccine.
People like myself who got the flu shot at the earliest date it was being offered were immunized against those strains.
Now, however, STAT has reported that concern has been raised about whether those were the best choices. This is because the Southern Hemisphere meeting determined that the H3N2 and B/Victoria strains do not match the dominant strains now circulating. The story quotes Danuta Skowronski, an influenza epidemiologist who described the situation as a “mismatch.”
It is not yet clear what this means for this years’ flu season in the U.S., but signals from the flu season in the Southern Hemisphere accurately predicted the severity of the very severe 2017-18 season. Stay tuned.
Because immune defenses decline with age, seniors should receive either Fluzone, a high-dose vaccine (four times the antigen compared with standard-dose) or Fluad, a vaccine with an adjuvant, MF59, that enhances the immune response.
Flublok is a recombinant vaccine that is produced without the use of the influenza virus or chicken eggs. It contains three times as much flu antigen as standard-dose vaccines and has been shown to reduce the chance of getting the flu by about 30% when compared to the standard dose inactivated vaccine.
Children between the ages of 6 months and 8 years old, who are getting vaccinated for the first time or who have not had at last 2 prior doses of a tri- or quadrivalent vaccine before July 1, 2017, should receive 2 doses of any inactivated vaccine at least 4 weeks apart. Otherwise, only one dose is required.
The flu can be more severe in pregnant women so they should definitely consider getting vaccinated. Although there was a concern during the 2010-2011 and 2011-2012 flu seasons that the flu vaccination could cause spontaneous abortion, a causal relationship has not been proven.1
Although the flu is an annoyance for most of us, it can be serious or even deadly in others. In fact, the flu is the most frequent cause of death from a vaccine-preventable disease in the United States.
Somewhere between 200,000 to 710,000 people are hospitalized and 12,000 to 56,000 die each year because of the flu and its complications, particularly pneumonia. Infants, people over 65, and those with chronic illnesses are at particular risk.
See the section on Treatment to learn about high-risk conditions.
There are three major reasons why people die from the flu:
A major change in the character of the virus antigens occurs periodically. This is known as an antigenic shift. When it occurs, the population may not have any pre-formed antibodies from prior infections and there often isn’t a vaccine. Because of this, a large number of people may be infected as the virus moves through the population. This is known as a pandemic.
The most severe pandemic in modern times occurred in the 1918-19 flu season. It is often called the Spanish flu. More than 500 million people were infected worldwide and an estimated 20 to 50 million people died in that pandemic.
Since then, there have been 5 other pandemics, the most recent in North America was in March 2009. The 2017-18 flu season, although not yet labeled a pandemic, was nevertheless considered a high severity season. The prevalence was close to that of the 2009 season.
This post was originally published on 10/18/17. It was updated on 10/19/19 to reflect the latest information on the 2019-2020 flu season.


El Baja Health Cluster formo parte de la Comitiva de Promoción del Sector Salud que visito Las Vegas, acompañando al...

Add the items of your interest in your planner, you can delete or add items anytime. The heart at the right corner shows the amount of items in your planner.
Submit your name, email and additional information you need about the providers. Our Concierge will send you all the information you need.
Address: Mision de Santo Tomas 2812, Zona Urbana Rio (4,69 km)
Tijuana
Available from 9:00 am – 19:00 pm